When you’re first diagnosed with diabetes, the news often comes as a shock. Even for patients whose family members have had diabetes, adjusting to a new lifestyle takes time and some research. Over the last year, we’ve answered many of your questions and provided a lot of diabetes education through articles on our website. To make it easier to find, we’ve compiled all these articles in one location. Feel free to bookmark this page. We’ll add links to new articles as we write them. If you have questions we haven’t answered here, leave us a note in the comments, ask one of our providers or comment on Facebook. We’d love to write more articles based on your questions.
Need information about diabetes? Start here:
How Your Provider Diagnoses Diabetes
Five Diabetes Symptoms You Can’t Ignore
How to Protect Your Feet with Diabetes
Six Ways to Manage Your Diabetes at Work
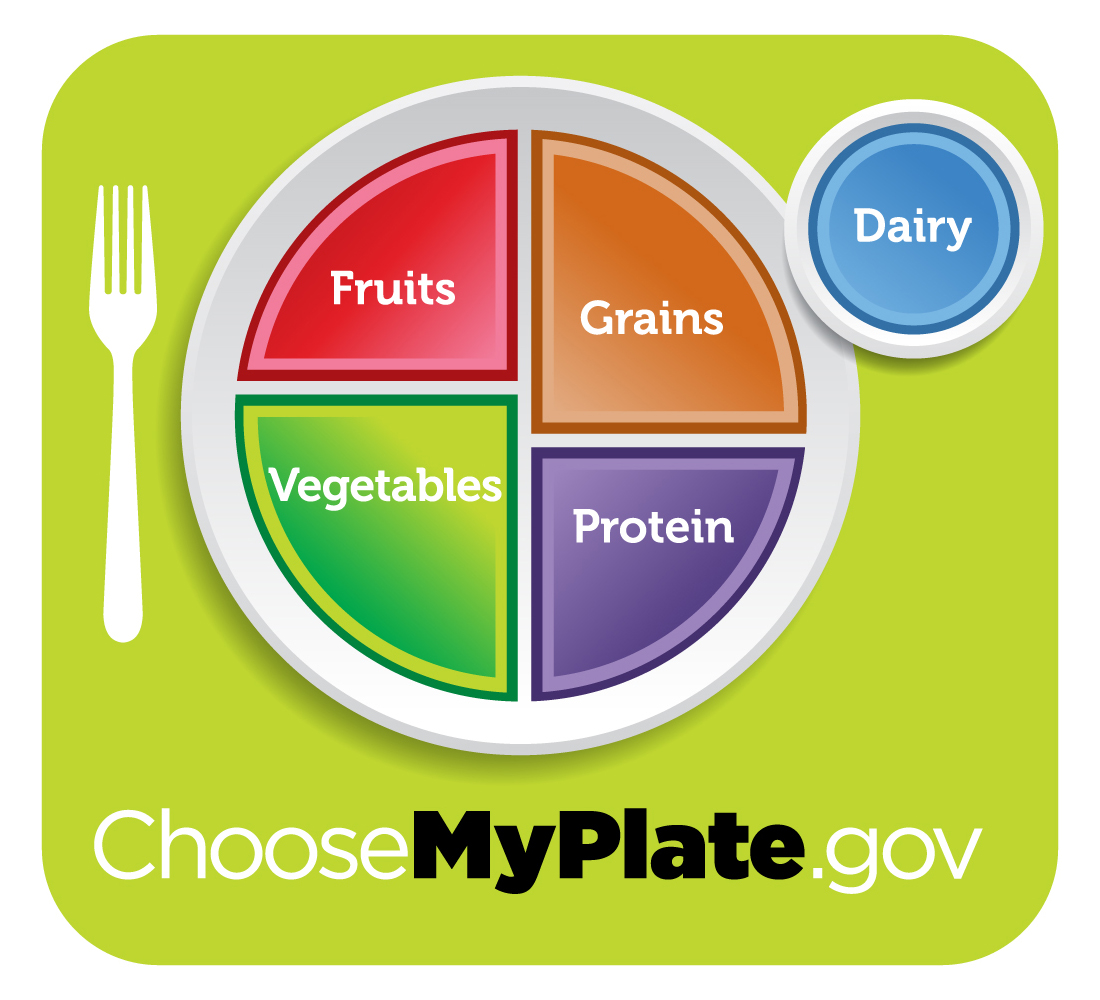
Best Breakfast Ideas for Diabetics
Sick Day Guidelines for People with Diabetes
Finding and Educating Your Diabetes Support Team
Diabetes and Your Vision: Risks, Symptoms, and Treatment
Diabetes and Heart Disease: A Deadly Duo