Let’s talk about post-traumatic stress disorder, or PTSD, as it’s better known. Like other mental health illnesses, PTSD has gained some myths since it was first discovered. We’re here to bust those myths wide open so you can understand the truth about PTSD. Check out our six PTSD myth busters.
PTSD Myth #1: PTSD only affects veterans.
Formerly referred to as “shell shock”, doctors initially associated PTSD with soldiers returning from war. However, the term changed when “post-traumatic stress disorder” first appeared in the third edition of the Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association in 1980. This change reflected a new understanding of PTSD. As mental health studies progressed, experts recognized common symptoms of shell shock in civilian patients who had experienced other types of physical and psychological trauma in their lifetime. PTSD better represented the broader circle of patients suffering from the same disorder.
PTSD Myth #2: PTSD develops immediately after trauma.
The truth is, PTSD can take weeks, months, or even years for symptoms to appear. Researchers have determined this is due to how the mind processes trauma and develops responses to fear. The typical time it takes for PTSD to manifest is three months but it’s not unusual for symptoms to appear years later.
PTSD Myth #3: PTSD only affects certain types of trauma victims.
People often associate PTSD with war veterans and those who have experienced traumatic events like abuse, serious accidents, or have been witnesses or victims of crime. However, trauma of any kind, including trauma from an illness, can cause PTSD. People who have been traumatized by an illness or injury may have anxiety related to healthcare because they associate doctor’s visits and hospitals with their ailment.
PTSD Myth #4: PTSD is not related to Traumatic Brain Injury (TBI).
Although the two conditions are not the same–Traumatic Brain Injury is an actual physical injury to the brain, commonly known as a concussion–they are, in some cases, related. Post-traumatic stress disorder can develop from TBI and symptoms of these conditions often overlap. When a possible TBI is involved in a PTSD case, diagnosis can prove difficult because evidence of physical trauma isn’t always apparent in diagnostic tests.
PTSD Myth #5: PTSD affects everyone who experiences trauma.
Actually, PTSD affects a relatively small group of trauma victims. PTSD rates are higher in women and other factors can make certain people more vulnerable to mental disorders. Risk factors include:
- Low self-esteem
- Low social support
- Multiple traumatic events
- More negative life events than usual
PTSD Myth #5: PTSD is for the weak.
The responses and behaviors of PTSD are of no fault of the person experiencing it, nor is the development of PTSD. PTSD is the brain’s way of trying to protect the person from more trauma. Hence, why responses like flight or fight are common. However, nothing about PTSD indicates the person is somehow “weaker” than others.
PTSD Myth #6: Symptoms of PTSD are the same in everyone.
PTSD can manifest in a number of ways. Some people experience intrusive thoughts about their trauma. Others may actively avoid thoughts, people, and places that remind them of their experiences. Arousal symptoms, such as difficulty sleeping or concentrating and being easily startled, are also common. Negative thoughts and moods are also other symptoms.
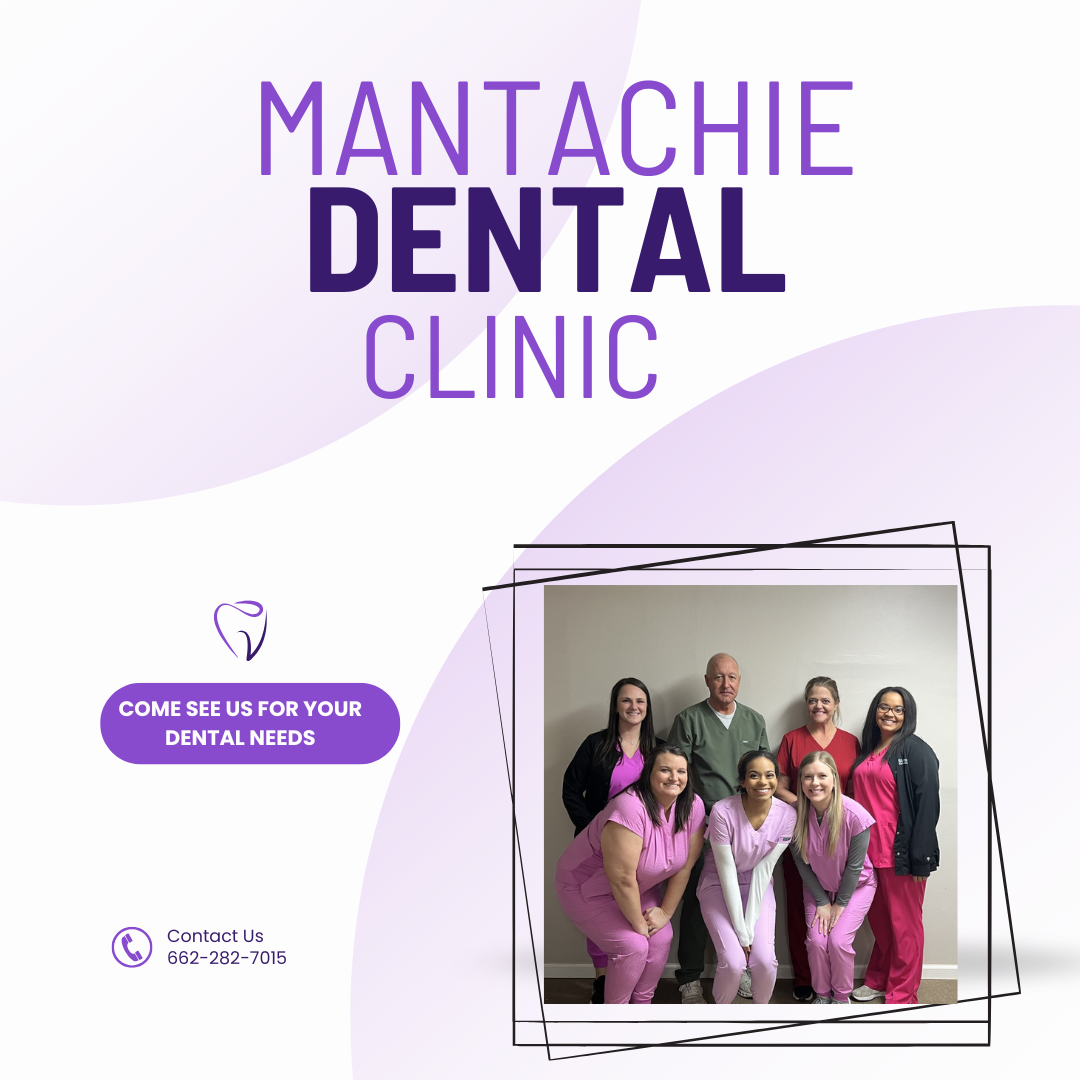
Are you concerned that you or someone you love is experiencing PTSD? Our behavioral health specialists can help. Contact Mantachie Rural Healthcare at 662-282-4226.




Speak Your Mind