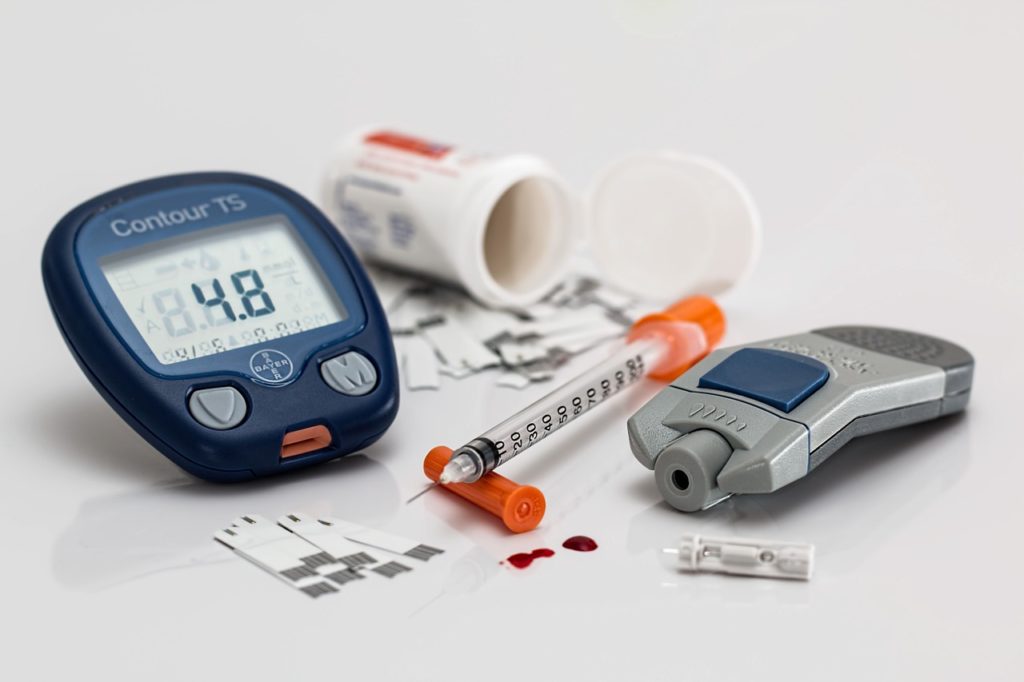
Lifestyle changes will most likely be the first suggestion your doctor makes after your type 2 diabetes diagnosis. The thought of changing your eating habits, adding exercise into an already full schedule, and monitoring your blood sugar can be overwhelming. Depending on how high your A1C is, your doctor may prescribe one of these common diabetes medications.
Type 1 and Type 2 diabetics take different types of medication because the types respond differently to insulin. Most Type 2 diabetes patients control their diabetes through oral medication.
Not all diabetes medication is right for every patient. Your doctor prescribes the type of medication based on your symptoms and how well your diabetes is controlled. Every addition of medication to your routine comes with questions you should ask your provider if they don’t supply the answer to these questions when they suggest the medication. Your pharmacy provided printouts contain most of this information, but talking to your doctor about these questions should still be the first step.
- When and how often should you take the medication?
- What should you do if you miss a dose?
- What are the common side effects of this medication?
- Why did your provider prescribe this particular medication?
- Will Medicare, Medicaid, or your private insurance cover this medication?
- Will this medication react with any other medications I’m taking?
Below are several of the most common Type 2 diabetes medications. We included a little information about each one. You can find more about these medications rxlist.com.
Metformin
Many providers prescribe metformin as the first medication for treating Type 2 diabetes. These medications help your body become more sensitive to insulin. They also decrease the amount of sugar your intestines absorb. It comes with side effects such as weight gain and possibly low blood sugar. Metformin is in a family of drugs called biguanides and may be combined with other medications also used to treat Type 2 diabetes.
Sulfonylureas
These medications stimulate the pancreas to make more insulin. Like Metformin, the side effects may include weight gain and low blood sugar.
Meglitinides
Like Sulfonylureas, these medications stimulate your pancreas to make more insulin, but they are faster acting and the effect lasts for a shorter length of time. These medications may lower your blood sugar too much.
Thiazolidinediones
These medications work a lot like Metformin in that they make your body more sensitive to glucose. Unfortunately, they come with more serious side-effects such as an increased risk of heart failure, heart disease, and anemia. Your provider will monitor your heart function closely if you take one of these medications. The increased risk of serious side effects means it probably won’t the first medication your provider prescribes.
DPP-4 inhibitors
These medications have less of a tendency to cause low blood sugar while helping the body make more insulin. They may cause joint pain and increase your risk of pancreatitis.
GLP-1 receptor agonists
This family of drugs slows digestion and helps lower blood sugar levels. They are injectable medications versus oral medications most often used. Patients with certain heart disease or chronic kidney disease are more likely to receive these medications as they may reduce the risk of heart attack and stroke. The medications often cause weight loss and may also have side effects like nausea and an increased risk of pancreatitis.
SGLT2 inhibitors
Unlike other diabetes medications, these drugs prevent the kidney from holding on to the glucose. Instead, your body excretes the sugar through your urine. These medications may also reduce the risk of heart attack and stroke. Possible side effects include vaginal yeast infections, urinary tract infections, low blood pressure, and a higher risk of diabetic ketoacidosis.
Insulin
Insulin was once the last resort for treating type 2 diabetes, but today it’s prescribed earlier due to its benefits. This medication must be injected. Your provider has a variety of types of insulin available, and they may prescribe a mixture of insulin types for use at different times of the day or night.
Cost of Medications
The cost of insulin and other diabetes medication continues to rise, and Medicare, Medicaid or your insurance may not cover all these medications. Patients at Mantachie Rural Health Care may request a 340B card at the time of their appointment for discounts on prescriptions. Discounts vary, but Fulton Walmart, Mantachie Pharmacy, and Saltillo Pharmacy and Solutions accept the cards.