The opening of a school-based health clinic in November at Mantachie schools represented more than a year’s worth of work. The clinic, staffed by Amy Floyd, FNP-C, and Casey Pounds, MA, sees both children and school staff. Hours of operation run from 7:30 a.m. until 3 p.m. during school days.
School-based health centers started in 1970, but gained popularity in the 1990s. Today, more than 2000 SBHCs care for the health of more than two million students.
Students with access to school-based clinics miss fewer days of school due to illness. More days in the classroom along with better overall health means these students retain more knowledge and score better on tests.
Parents benefit from school-based clinics because they miss fewer days of work to attend appointments with their children. Increased work attendance and productivity improves a family’s financial outlook.
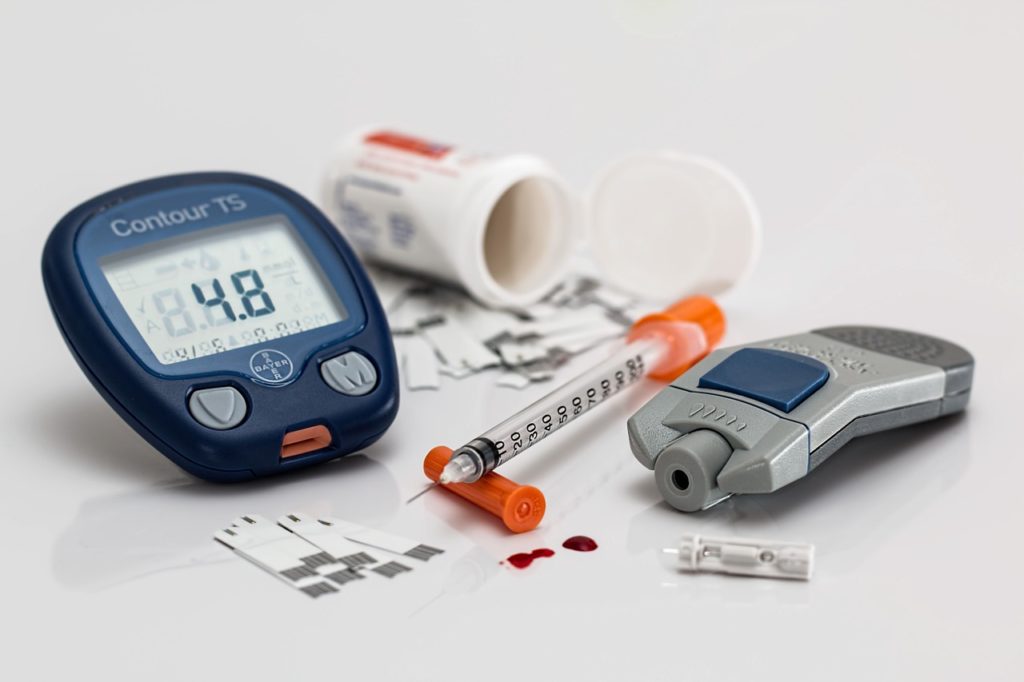
Our school-based clinic treats the usual urgent care illnesses such as colds, sinus infections, strep throat, and the flu, as well as managing health conditions like diabetes. Providers may also conduct vision and hearing screenings for students. Students experiencing depression or other mental illness may receive earlier intervention when a medical provider is on campus every day.
The benefits of consistent health care for students stretch into a lifetime of healthy choices, which benefits the entire family and community.
To be seen in the school-based clinic, parents and staff must complete the permission and insurance form available in the school office. The clinic bills visits to the student’s Medicaid or private insurance.