Most of the time when our medical provider talks about bacteria and our body it’s not a good thing. When it comes to the naturally occurring bacteria in your stomach, it looks like more can be better.
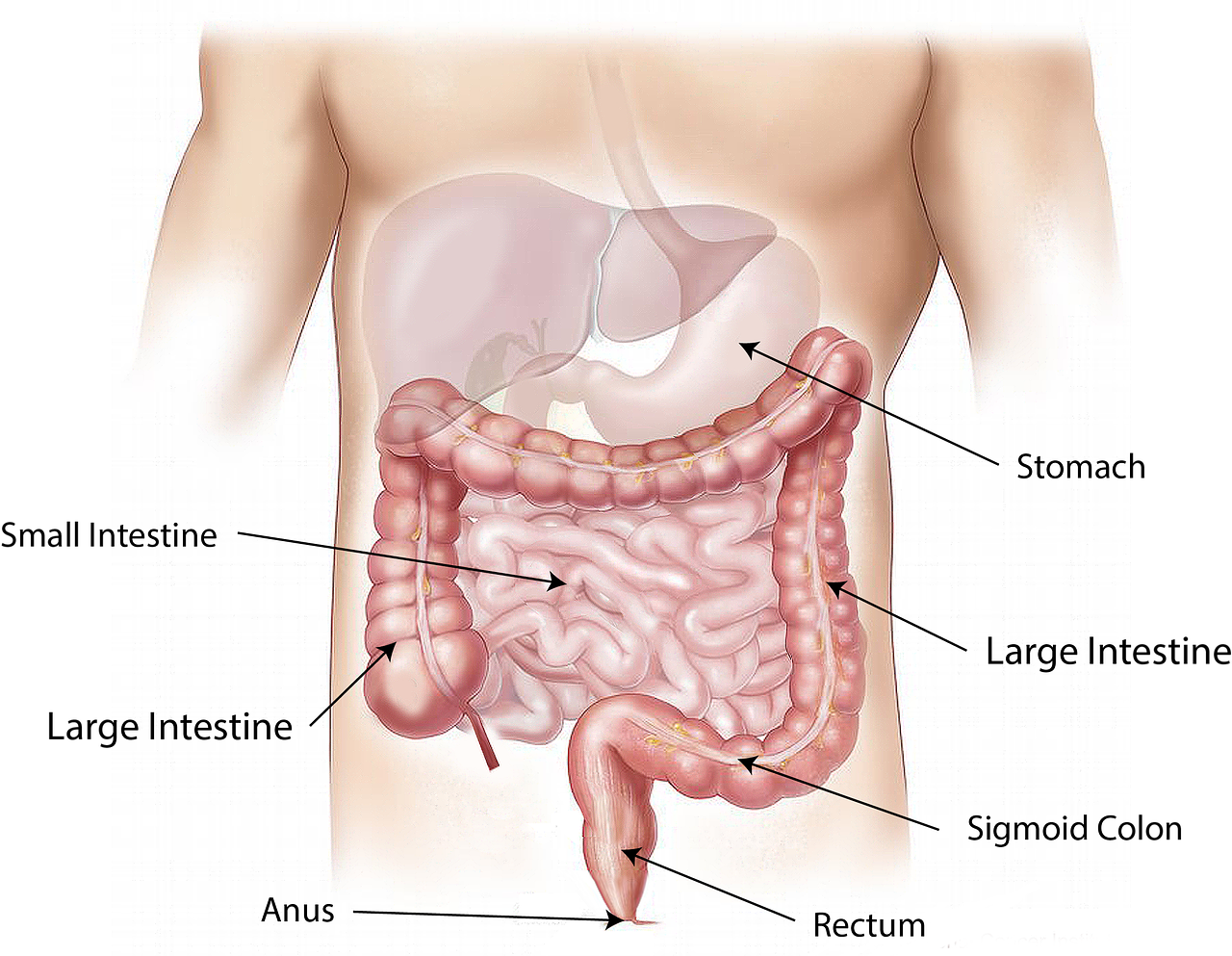
Somewhere between 300 and 500 different kinds of bacteria live in our intestines, and that’s a good thing. These bacteria work with other tiny organisms to make up the microbiota in our intestines. Researchers call the gut our “second brain”. The microbiota in our gut affects everything from our metabolism to our mood to our immune system.
Gut Bacteria Linked to Chronic Illness
Research into this gut bacteria shows differences between the types of bacteria in healthy people versus those with certain illnesses. While it makes sense what’s happening in our gut would affect chronic diseases such as colon cancer or Crohn’s disease, gut bacteria may also increase your chances for heart disease, type 2 diabetes, depression, anxiety, autism, and rheumatoid arthritis.
How to Encourage Good Bacteria Growth
What goes into our bodies affects how our bodies work. Encourage good gut bacteria by eating a nutritious diet high in fiber-rich foods. Processed foods and diets filled with red meats can kill certain gut bacteria. Having a variety of gut bacteria appears in research to be as important as having a lot of good gut bacteria.
Exercise can also increase the variety of gut bacteria so aim for 30 minutes of exercise at least five times a week. We’ve discussed the importance of exercise in controlling blood pressure, reducing heart disease and managing type 2 diabetes. All those illnesses may have some link to gut bacteria which can be affected by exercise.
Finally, only take antibiotics when your provider determines it’s necessary. Antibiotics will not help your cold or flu. Those viruses must run their course. Antibiotics not only kill the bad bacteria but the good gut bacteria your body needs.
Research is on-going to determine how certain gut bacteria affect disease and what we can do to increase it in our intestines. If you’d like to learn more about gut bacteria and the research surrounding it, we found this article by WebMD to be especially helpful.








 Ben Napier and his wife Erin, both Mississippi natives and graduate of Ole Miss, host the HGTV show
Ben Napier and his wife Erin, both Mississippi natives and graduate of Ole Miss, host the HGTV show 
