Every year with the “New Year New You” announcements come new fad diets. One of the most popular new celebrity-touted trends is intermittent fasting. Most notably a 16:8 fast. Fasting has been around for centuries, but it’s not right for everyone.
What is fasting?
Before you consider fasting as part of your diet and exercise plan, educate yourself on the different types of fasting. Religious fasts often include not eating for many days or even weeks at a time. This type of fasting can be particularly dangerous for people with diabetes.
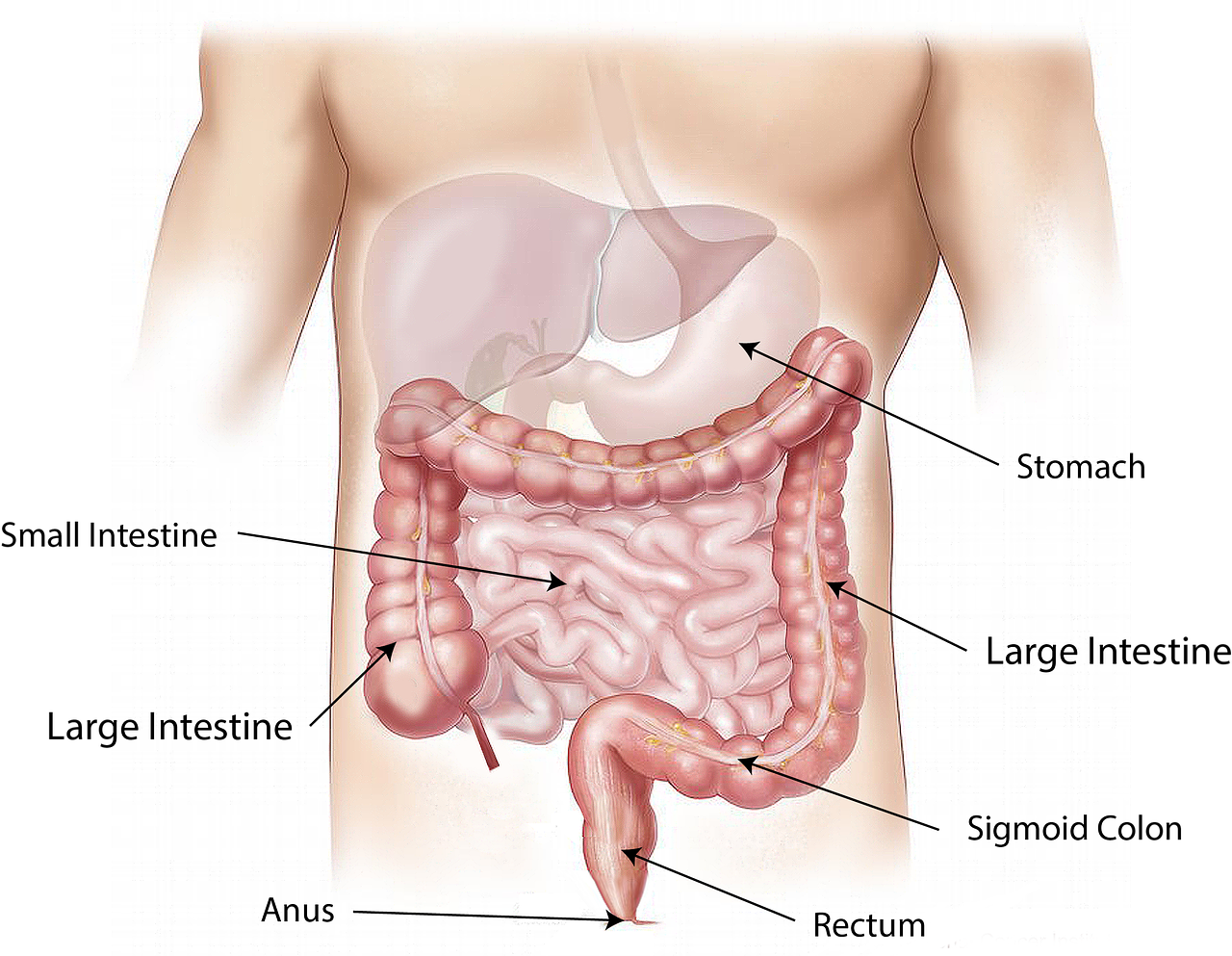
Intermittent fasts are broken down by when you restrict food intake. A 5:2 fast allows you to eat your regular diet five days a week and restricts calories to 600 calories a day for men and 500 calories for women on the two fasting days. The popular 16:8 fast means you fast for 16 hours a day and eat all your daily calories in the remaining 8 hours.
Benefits of Intermittent Fasting
Some dieters find the freedom of eating regular meals five days a week makes up for two days of strict fasting, or that they aren’t really all that hungry when they eat three meals in eight hours instead of stretching out their meals and snacking over the entire day. The diet plan is easy to follow because it doesn’t include any measuring of food or counting of calories.
A few very limited studies have shown intermittent fasting to lower A1C levels and increase weight loss.
Dangers of Intermittent Fasting
Every diet has pros and cons. Intermittent fasting may help prevent type 2 diabetes, but it’s not a good option for those who already have the disease. Fasting may cause lower blood sugar levels, which can have dangerous side effects.
Because intermittent fasting does not involve measuring serving sizes or counting calories, many people will gorge on the foods they love or eat unhealthy foods during their non-fasting days.
Fasting may also be dangerous for people with a history of eating disorders or mental health disorders.
Good Eating Habits Haven’t Changed
Regardless of whether you try eating all your meals in one eight hour stint or not, what you put in your mouth matters. Filling your plate with fruits and vegetables, adding lean protein, substituting complex carbs in place of sugary carbs, and including a few healthy fats helps you lose weight and manage diabetes and other medical conditions. The limited studies show no greater weight loss in groups who fasted than from groups who ate regular, healthy meals.
Before You Try Any Diet
Always consult your medical provider before you start any new diet or exercise routine. Your personal health conditions and medications influence how exercise and diet affect your body. We have a nutritionist on staff who can help you find the best way to manage your diet so it has the most positive effect on your health. She hosts Witcher’s Weightloss Warriors every Monday evening. It’s a free program that teaches participants how to lose weight in healthy ways. Call our clinic to learn how you can join.